How To Check for DVT At Home
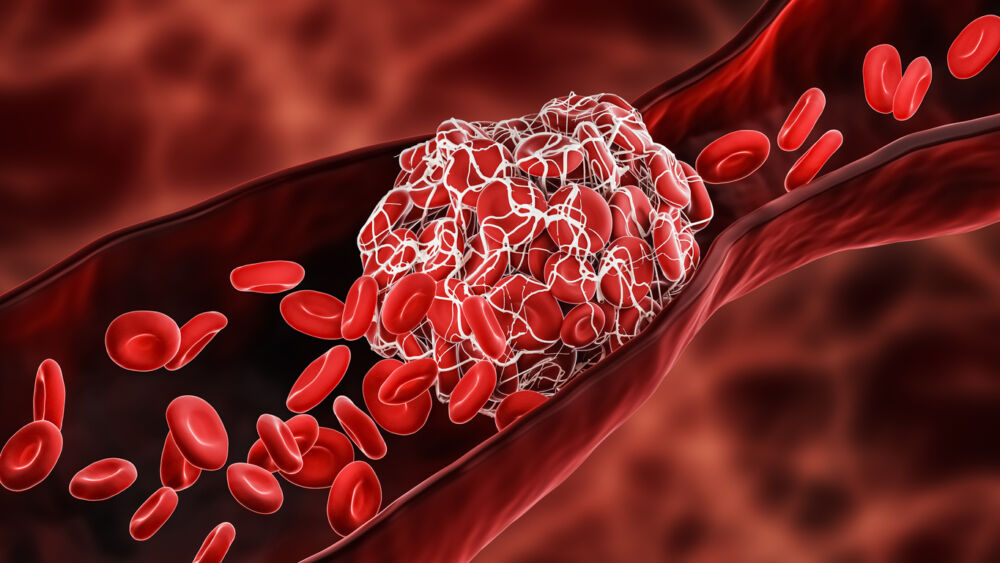
Deep Vein Thrombosis are a potentially life threating medical condition. Here are some of the symptoms of a DVT to be aware of and a quick test you can do at home.

Vein physician and chronic venous insufficiency (vein disease) expert Peter J. Pappas, MD, FACS, is a Vascular Surgeon and Director of the Venous and Lymphatic Fellowship Program at Center for Vein Restoration. He is the lead physician at Center for Vein Restoration center locations in Union, New Jersey, and Morristown, New Jersey.
Leg pain is a common complaint. Because lower extremities are made up of a complex arrangement of muscles, joints, nerves, ligaments, tendons, and blood vessels, the cause of leg pain can sometimes be difficult to pinpoint.
That's why we spoke to an expert, vein specialist Dr. Peter Pappas, about how to distinguish between different kinds of leg pain. Learn what type of doctor treats various types of leg pain and when leg pain requires immediate medical attention.
Dr. Pappas points to the COVID-19 pandemic as giving rise to confusion between vein-related and non-vein-related leg pain. Pointing to inactivity during lockdown, as people get out and move more, complaints of leg pain have become commonplace.
Those suffering from leg pain are often confused about the root cause of their pain and, as a result, seek out the wrong kind of help or the wrong kind of doctor.
This article seeks to clear the confusion by identifying the symptoms and causes of venous-related and non-venous-related leg pain—and direct patients to the correct practitioner for care.
“Lately, in the post-COVID patient, we see people who have been sitting at home without being ambulatory… When they start to get back to normal activities, they tend to get muscular-type pain. They mistake muscle pain for a blood clot because they’ve heard that having COVID or a flu vaccine is associated with blood clots. However, 99 percent of the time it is not a blood clot. Patients are simply using muscles they haven’t used in a while and are experiencing muscle related discomfort.” – Dr. Peter J. Pappas
Venous insufficiency (vein disease) is the failure of the veins to adequately circulate the blood in the lower extremities due to improper functioning of the vein valves in the legs.
According to Dr. Pappas, patients suffering from vein-related pain experience tired, heavy, achy legs that get worse with prolonged standing or sitting, leg cramps (especially at night), and feelings of restless legs.
Vein-related leg pain gets worse by the end of the day and can be associated with leg swelling.
Yes. Dr. Pappas says that 98 percent of patients who come to him about itchy, hot, painful spider veins are women and symptoms are often worse around the time of a woman’s menses.
He explains that, unfortunately, insurance companies don’t consider spider veins to be “symptomatic varicosities.” In other words, insurance considers spider veins a cosmetic issue.
Dr. Pappas adds, “at Center for Vein Restoration, spider vein treatment is inexpensive. We can take care of spider veins at a very low cost to the patient.”
A vein specialist will have the patient undergo an ultrasound from the groin to the ankle to ensure there is no blood clot and to assess vein function. Center for Vein Restoration offers many minimally invasive, in-office treatment options based on the patient’s history, physical exam, and quality of life impairment. Insurance will cover treatment if the disorder meets their specific insurance carrier’s criteria.
Leg pain can have causes that are not related to vein disease. In these cases, physical activity, lack of activity, overuse injury in the muscles, ligaments, tendons, bones or joints, sprains, or problems in the lower spine are possible causes.
Dr. Pappas recommends that people seek medical care from a primary care physician, orthopedic doctor, vascular surgeon, or other medical professional if they experience the following:
Sciatica is pain that moves along the sciatic nerve from the lower back and shoots down one or both legs. This is usually caused when a herniated disk, spasm of a muscle under the buttocks, or bone spur in the spine that presses on the nerve.
Dr. Pappas describes pain caused by nerves or sciatica as “beginning in the lower back or buttocks and extending to the side of the leg and into the calves. In particularly bad cases, this pain can extend into the foot, in-between the first and second toe, and down to the bottom or sole of the foot. It sometimes includes a burning sensation or electric shock feeling which indicates nerve or sciatica pain.”
Dr. Pappas defines another type of non-vein-related pain, specifically muscular pain, as “pinpoint pain.” When muscular or tendonitis issues are the origin of leg pain, a patient can point to the spot, usually on the back of the thigh or the side of the legs near the knee. Muscular or tendonitis pain and muscle strain is different from other pain because it usually gets worse with movement.
Pain or swelling isolated to a joint is usually not vein-related and is most often associated with arthritis. Vein-related pain is more global and not isolated to the knee, ankle, or hip.
Unlike vein-related pain, arterial pain from disruption of blood flow is limb and life-threatening and can increase one’s risk for a heart attack or stroke. While arterial pain can happen at rest, pain in the thigh, calf, or buttocks during ambulation eases when the person stops walking and rests.
The pain is reproducible over a specific distance and decreases over five to 15 minutes with rest. Once the pain dissipates, the patient can walk the same distance with the development of pain in the same muscle groups.
Neurogenic claudication caused by compressed nerves in the lower spine is only relieved when the person sits. Patients have good days and bad days with variable distances they can walk before the onset of pain.
People with suspected arterial claudication must seek an immediate evaluation from a vascular specialist.
Dr. Pappas emphasizes that “vein disease is not limb-threatening nor life-threatening and is specifically a quality-of-life issue.” He recommends that a person seek medical attention from a vein doctor if symptoms affect their quality of life. These issues include tired, heavy, achy legs, pain associated with prolonged standing, pain that is worse at the end of the day, and leg swelling that requires elevation or getting off their legs.
Dr. Pappas cautions: never allow vein problems as listed above to get to the point that skin becomes damaged or that wounds form.
Call 240-965-3915 or visit centerforvein.com for additional information or to schedule an appointment. Treatment is covered by most major insurance providers, including Medicare and Medicaid.